Colonoscopy & Flexible Sigmoidoscopy

What is a Colonoscopy?
A colonoscopy is an investigatory procedure that allows your surgeon to examine the rectum, colon and a distal portion of the small intestine (terminal ileum). It is performed using a device called a colonoscope, which is a long flexible tube containing a camera and a light that is passed through the anus into the lower gastrointestinal tract.
What is a Flexible Sigmoidoscopy?
A flexible sigmoidoscopy is an investigatory procedure that allows your surgeon to examine the rectum and the distal segment of the large bowel (sigmoid colon and descending colon). It is performed using a device called a sigmoidoscope, which is a short flexible tube containing a camera and light that is passed through the anus into the rectum, sigmoid and descending colon.
This procedure is done under sedation and hence no pain or discomfort to the patient.
The investigation is done as day procedure and the patient will able to go home on the same day.
The patient will be advised to refrain from driving or serious work for 24 hours.
A colonoscopy is commonly indicated if you have:
- A positive faecal occult blood test
- Rectal Bleeding
- Change in bowel habits
- Past history of bowel cancer or polyps
- Family history of bowel cancer
- Weight loss or loss of appetite
- Iron-deficiency anaemia
- Abnormal imaging studies
A flexible sigmoidoscopy is indicated if:
- Rectal Bleeding
- Past history of rectal cancer or polyps
- Persistent diarrhoea
- Management of inflammatory bowel disease
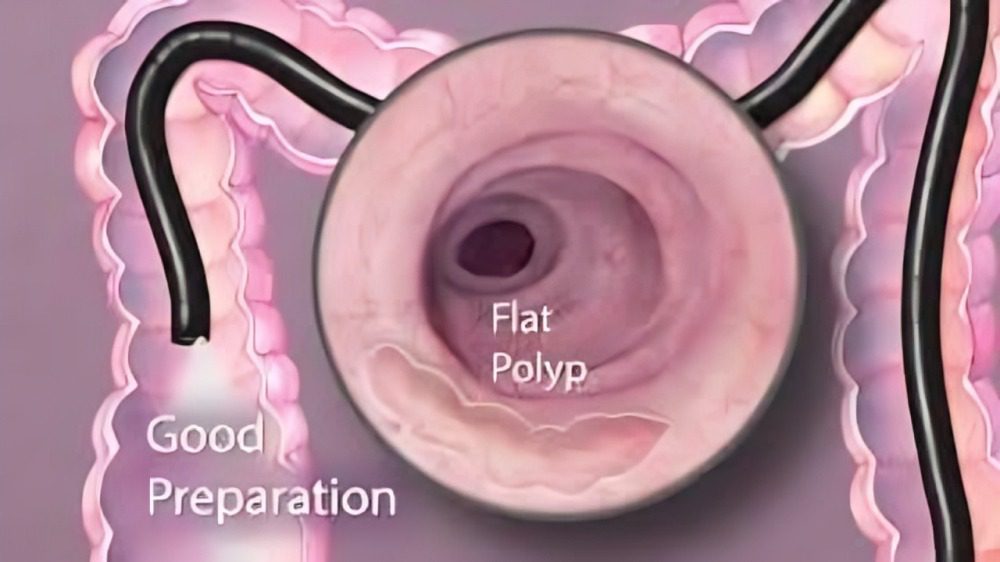
Preparation
Most of the patients will have a consultation before the procedure. If the patient is busy or unable to come we could organise the procedure as an open access colonoscopy. This means the patient will be given all the information over the phone and the surgeon will talk to the patient at the day of the procedure.
If you are undergoing a colonoscopy, our clinic will provide you with an information package detailing the preparation. A colonoscopy requires a course of bowel preparation to ensure the large bowel is clear to detect any abnormalities. If you have any questions regarding the bowel preparation for colonoscopy, please contact our clinic. Please advise us if you are on anti-platelets, anticoagulants, diabetic medications and any significant medical history prior to the procedure.
If you are undergoing a flexible sigmoidoscopy, just prior to the procedure you will receive an enema to ensure a clear view of the lower gastrointestinal tract. This will be arranged for you by the hospital. Flexible sigmoidoscopy does not require a course of bowel preparation.
The Procedure
Prior to the procedure, the anaesthetist will provide you with sedation and analgesia to help you feel relaxed and settled during the colonoscopy. The given sedation will cause you to fall asleep during the colonoscopy so that you do not experience discomfort or pain during the procedure.
You will be asked to lie on the left-hand side of the bed with your knees drawn up to your chest. The scope will then be gently inserted through the anus into the rectum and a small amount of carbon dioxide is introduced to allow inflation of the colon for a better view. The scope will then be advanced through the large bowel up to the distal portion of the small intestine in a colonoscopy. In flexible sigmoidoscopy, the scope will only be advanced up to the descending colon, which is the lower portion of your large bowel. Your doctor will carefully inspect the mucosal lining of your colon as the scope is withdrawn. Photographs will be taken inside of the colon will be taken for documentation and reporting.
A colonoscopy can detect:
- Colorectal polyps and cancer
- Inflammatory change in bowel
- Ulceration in the mucosa
- Polyps, which can then be removed
- Diverticulosis
- Colonic strictures/narrowing
A flexible sigmoidoscopy can detect:
- Distal colonic or rectal polyps and cancer
- Inflammatory or ulcerative changes in the distal colon
- Haemorrhoids
If an abnormal or inflammatory area of colonic mucosa is seen during the procedure, the surgeon will perform a biopsy or removal of this lesion. It will then be sent for examination to identify any pathology.
If a polyp is seen during the procedure, the polyp will be removed and it will then be sent for examination to identify any pathology or cancerous changes.
The entire procedure can take up to 15-30 minutes. You will be discharged from the hospital on the same day.